Dioum, E. M., Schneider, K. L., Vigerust, D. J., Cox, B. D., . . . Furman, D. (2022). Oats lower age-related systemic chronic inflammation (iAge) in adults at risk for cardiovascular disease. Nutrients, 14(21), 4471. doi:10.3390/nu14214471
Abstract:
Despite being largely preventable, cardiovascular disease (CVD) is still the leading cause of death globally. Recent studies suggest that the immune system, particularly a form of systemic chronic inflammation (SCI), is involved in the mechanisms leading to CVD; thus, targeting SCI may help prevent or delay the onset of CVD. In a recent placebo-controlled randomized clinical trial, an oat product providing 3 g of β-Glucan improved cholesterol low-density lipoprotein (LDL) levels and lowered cardiovascular risk in adults with borderline high cholesterol. Here, we conducted a secondary measurement of the serum samples to test whether the oat product has the potential to reduce SCI and improve other clinical outcomes related to healthy aging. We investigated the effects of the oat product on a novel metric for SCI called Inflammatory Age® (iAge®), derived from the Stanford 1000 Immunomes Project. The iAge® predicts multimorbidity, frailty, immune decline, premature cardiovascular aging, and all-cause mortality on a personalized level. A beneficial effect of the oat product was observed in subjects with elevated levels of iAge® at baseline (>49.6 iAge® years) as early as two weeks post-treatment. The rice control group did not show any significant change in iAge®. Interestingly, the effects of the oat product on iAge® were largely driven by a decrease in the Eotaxin-1 protein, an aging-related chemokine, independent of a person’s gender, body mass index, or chronological age. Thus, we describe a novel anti-SCI role for oats that could have a major impact on functional, preventative, and personalized medicine.
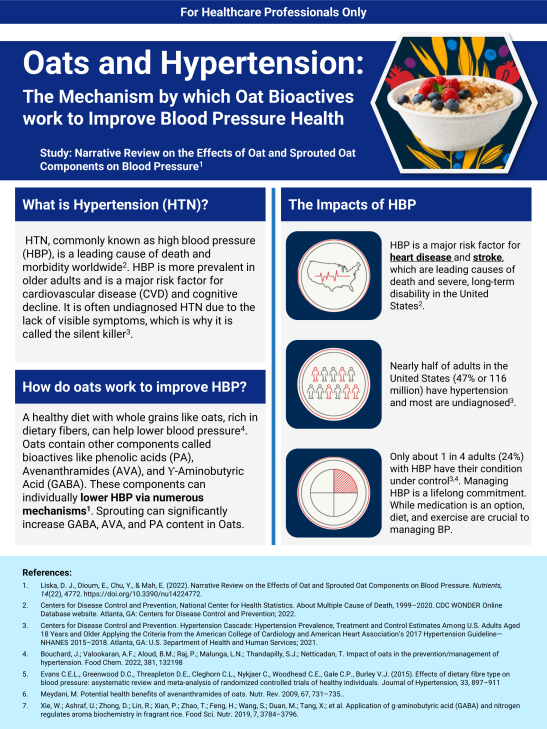
Liska, D. J, Dioum, E., Chu, Y., Mah, E. (2022). Narrative review on the effects of oat and sprouted oat components on blood pressure. Nutrients, 14(22), 4772. doi:10.3390/nu14224772
Abstract:
Hypertension (HTN) is a major risk factor for cardiovascular disease (CVD) and cognitive decline. Elevations in blood pressure (BP) leading to HTN can be found in young adults with increased prevalence as people age. Oats are known to decrease CVD risk via an established effect of β-glucan on the attenuation of blood cholesterol. Many past studies on CVD and oats have also reported a decrease in BP; however, a thorough assessment of oats and BP has not been conducted. Moreover, oats deliver several beneficial dietary components with putative beneficial effects on BP or endothelial function, such as β-glucan, γ-amino butyric acid (GABA), and phytochemicals such as avenanthramides. We conducted a comprehensive search for systematic reviews, meta-analyses, and clinical intervention studies on oats and BP and identified 18 randomized controlled trials (RCTs) and three meta-analyses that supported the role of oats in decreasing BP. Emerging data also suggest oat consumption may reduce the use of anti-hypertensive medications. The majority of these studies utilized whole oats or oat bran, which include a vast array of oat bioactives. Therefore, we also extensively reviewed the literature on these bioactives and their putative effect on BP-relevant mechanisms. The data suggest several oat components, such as GABA, as well as the delivery of high-quality plant protein and fermentable prebiotic fiber, may contribute to the anti-HTN effect of oats. In particular, GABA is enhanced in oat sprouts, which suggests this food may be particularly beneficial for healthy BP management.
Wolever, T. M. S., Rahn, M., Duom, E. H., Spruill, S. E., . . . Chu, Y. (2021). An oat β-glucan beverage reduces LDL cholesterol and cardiovascular disease risk in men and women with borderline high cholesterol: A double-blind, randomized, controlled clinical trial. The Journal of Nutrition, 151(9), 2655–2666. doi:10.1093/jn/nxab154
Abstract:
Background High-molecular-weight (MW) oat β-glucan (OBG), consumed at 3–4 g/d, in solid foods reduces LDL cholesterol by a median of ∼6.5%. Objectives We evaluated the effect of a beverage providing 3 g/d high-MW OBG on reduction of LDL cholesterol (primary endpoint) when compared with placebo. Methods We performed a parallel-design, randomized clinical trial at a contract research organization; participants, caregivers, and outcome assessors were blinded to treatment allocation. Participants with LDL cholesterol between 3.0 and 5.0 mmol/L, inclusive [n = 538 screened, n = 260 ineligible, n = 23 lost, n = 48 withdrawn (product safety); n = 207 randomly assigned, n = 7 dropped out, n = 9 withdrawn (protocol violation); n = 191 analyzed; n = 72 (37.7%) male, mean ± SD age: 43.3 ± 14.3 y, BMI: 29.7 ± 5.2 kg/m2], were randomly assigned to consume, 3 times daily for 4 wk, 1 g OBG (n = 104, n = 96 analyzed) or rice powder (Control, n = 103, n = 95 analyzed) mixed into 250 mL water. Treatment effects were assessed as change from baseline and differences analyzed using a 2-sided t test via ANOVA with baseline characteristics as covariates. Results After 4 wk, change from baseline least-squares-mean LDL cholesterol on OBG (−0.195 mmol/L) was less than on Control (0.012 mmol/L) by mean: 0.207 mmol/L (95% CI: 0.318, 0.096 mmol/L; P = 0.0003); the following secondary endpoints were also reduced as follows: total cholesterol (TC) (0.226 mmol/L; 95% CI: 0.361, 0.091 mmol/L; P = 0.001), TC:HDL cholesterol ratio (0.147; 95% CI: 0.284, 0.010; P = 0.036), non-HDL cholesterol (0.194 mmol/L; 95% CI: 0.314, 0.073 mmol/L; P = 0.002), and Framingham cardiovascular disease (CVD) risk (0.474; 95% CI: 0.900, 0.049, P = 0.029). Changes in HDL cholesterol, triglycerides, glucose, and insulin did not differ between treatment groups (P > 0.05). Lipid treatment effects were not significantly modified by age, sex, BMI, or hypertension treatment. There were no major adverse events, but both treatments transiently increased gastrointestinal symptoms. Conclusions Consuming a beverage containing 1 g high-MW OBG 3 times daily for 4 wk significantly reduced LDL cholesterol by ∼6% and CVD risk by ∼8% in healthy adults with LDL cholesterol between 3 and 5 mmol/L.
Xu, D., Wang, S., Feng, M., Shete, V., . . . Yang, Y. (2021). Serum metabolomics reveals underlying mechanisms of cholesterol-lowering effects of oat consumption: A randomized controlled trial in a mildly hypercholesterolemic population. Molecular Nutrition & Food Research, 65(9). doi:10.1002/mnfr.202001059
Abstract:
Introduction The purpose of this study is to examine the effects of oat supplementation on serum lipid in a population of adults with mild hypercholesterolemia and reveal the underlying mechanisms with serum untargeted metabolomics. Methods and Results In this placebo-controlled trial, 62 participants from Nanjing, China, with mild elevations in cholesterol are randomly assigned to receive 80 g oats (containing 3 g beta-glucan) or rice daily for 45 days. Fasting blood samples are collected at the beginning, middle, and end of the trial. Compared with the rice group, oat consumption significantly decreases serum total cholesterol (TC) (-8.41%, p = 0.005), low-density lipoprotein cholesterol (LDL-c) (-13.93%, p = 0.001), and non high-density lipoprotein cholesterol (non-HDL-c) (-10.93%, p = 0.017) levels. There are no significant between-group differences in serum triglyceride (TG), apolipoprotein B (Apo B), glycated albumin, or fasting blood glucose levels. An orthogonal partial least squares discriminant analysis (OPLS-DA) suggests a clear separation in metabolic profiles between the groups after the intervention. Twenty-one metabolites in the oat group are significantly different from those in the rice group, among which 14 metabolites show a decreased trend. In comparison, seven metabolites show an increased trend. Correlations analysis from both groups indicate that most metabolites [e.g., sphinganine and phosphatidylcholine (PC)(20:5(5Z,8Z,11Z,14Z,17Z)/20:1(11Z))] have positive correlations with serum cholesterol levels. Kyoto Encyclopedia of Gene and Genomes pathway analysis suggests that oat consumption regulated glycerophospholipid, alanine, aspartate and glutamate, sphingolipid, and retinol metabolism. Conclusion Oat consumption has beneficial effects on serum lipids profiles. The underlying mechanisms involve glycerophospholipid, alanine, aspartate and glutamate, sphingolipid, and retinol metabolism in adults.
Xu, D., Feng, M., Chu, Y., Wang, S., . . . Yang, Y. (2021). The prebiotic effects of oats on blood lipids, gut microbiota, and short-chain fatty acids in mildly hypercholesterolemic subjects compared with rice: A randomized, controlled trial. Frontiers in Immunology, 12. doi:10.3389/fimmu.2021.787797
Abstract:
Phytochemicals derived from oats are reported to possess a beneficial effect on modulating dyslipidemia, specifically on lowering total and LDL cholesterol. However, deeper insights into its mechanism remain unclear. In this randomized controlled study, we assigned 210 mildly hypercholesterolemic subjects from three study centers across China (Beijing, Nanjing, and Shanghai) to consume 80 g of oats or rice daily for 45 days. Plasma lipid profiles, short chain fatty acids (SCFAs), and fecal microbiota were measured. The results showed that total cholesterol (TC) and non-high-density lipoprotein cholesterol (non-HDL-C) decreased significantly with both oats and rice intake after 30 and 45 days. The reduction in TC and non-HDL-C was greater in the participants consuming oats compared with rice at day 45 (p = 0.011 and 0.049, respectively). Oat consumption significantly increased the abundance of Akkermansia muciniphila and Roseburia, and the relative abundance of Dialister, Butyrivibrio, and Paraprevotella, and decreased unclassified f-Sutterellaceae. In the oat group, Bifidobacterium abundance was negatively correlated with LDL-C (p = 0.01, r = −0.31) and, TC and LDL-C were negatively correlated to Faecalibacterium prausnitzii (p = 0.02, r = −0.29; p = 0.03, r = −0.27,respectively). Enterobacteriaceae, Roseburia, and Faecalibacterium prausnitzii were positively correlated with plasma butyric acid and valeric acid concentrations and negatively correlated to isobutyric acid. HDL-C was negatively correlated with valeric acid (p = 0.02, r = −0.25) and total triglyceride (TG) was positively correlated to isovaleric acid (p = 0.03, r = 0.23). Taken together, oats consumption significantly reduced TC and LDL-C, and also mediated a prebiotic effect on gut microbiome. Akkermansia muciniphila, Roseburia, Bifidobacterium, and Faecalibacterium prausnitzii, and plasma SCFA correlated with oat-induced changes in plasma lipids, suggesting prebiotic activity of oats to modulate gut microbiome could contribute towards its cholesterol-lowering effect.
Fulgoni, V. L., Brauchla, M., Fleige, L., & Chu, Y. (2020). Association of whole-grain and dietary fiber intake with cardiometabolic risk in children and adolescents. Nutrition and Health, 26(3), 243-251. doi:10.1177/0260106020928664
Abstract:
Background: Diet is known to affect many risk factors of cardiovascular disease (CVD), a leading cause of mortality and morbidity. Aim: The objective of this study was to explore the potential association between whole grain and dietary fiber with CVD risk factors, including metabolic syndrome (MetS) in children and adolescents using National Health and Nutrition Examination Survey (NHANES) 2003–2014. Methods: Two days of 24-hour recall data from 16,507 children and adolescents age 2–18 years were used to estimate dietary intakes. Continuous MetS scores (cMetS) were computed by aggregating age/sex regressed z-scores of waist circumference, mean arterial blood pressure, high-density lipoprotein-cholesterol, triglycerides, and glucose. Regression analyses were used to assess association of fiber and whole grain intake with cardiometabolic markers including MetS after adjusting for demographic factors. Results: Increasing tertiles of fiber intake were significantly associated with 3% lowered risk MetS in adolescents age 13–18 years. Additionally, increasing intake tertiles of fiber were associated with reduced risk elevated cholesterol (5–11% reduction), elevated diastolic blood pressure (10–23% reduction) in adolescents age 13–18 years, and risk of obesity (3–5% reduction) in children and adolescent age 2–18 years. Increasing tertiles of whole grain intake were only associated with reduced risk of elevated triglycerides (52% risk reduction) in adolescents age 13–18 years. Conclusion: The results suggest that intake of dietary fiber was inversely associated with several markers of cardiovascular disease risk including MetS.
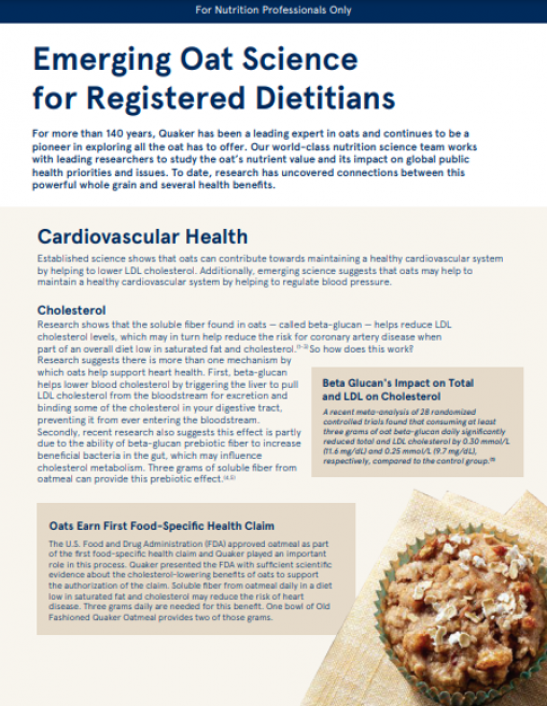
Mathews, R., Kamil, A., & Chu, Y. (2020). Global review of heart health claims for oat β-glucan products. Nutrition Reviews, 78(S1), 78-97. doi:10.1093/nutrit/nuz069
Abstract:
Coronary heart disease (CHD) is the leading cause of death globally. Consumption of whole grains and cereal fiber, as part of a healthy diet, can lower the risk of CHD. Health claims on food products are effective in helping consumers select healthful diets. The US Food and Drug Administration was the first to approve a health claim, in 1997, between β-glucan soluble fiber from whole oats, oat bran, and whole oat flour and reduced risk of CHD. Only a few countries have approved similar claims. Since 1997, a significant amount of additional evidence has been published on the relationship between oat β-glucan and CHD. To assist other jurisdictions in potentially utilizing this claim, the full extent of data that supports this claim (ie, the evidence utilized by the US Food and Drug Administration to substantiate the claim, as well as the results of 49 clinical trials published since 1997) are reviewed here. The complexities involved in authoring evidence-based health claims, including the impact of processing on β-glucan cholesterol-lowering efficacy in approving eligible β-glucan products, are also discussed.
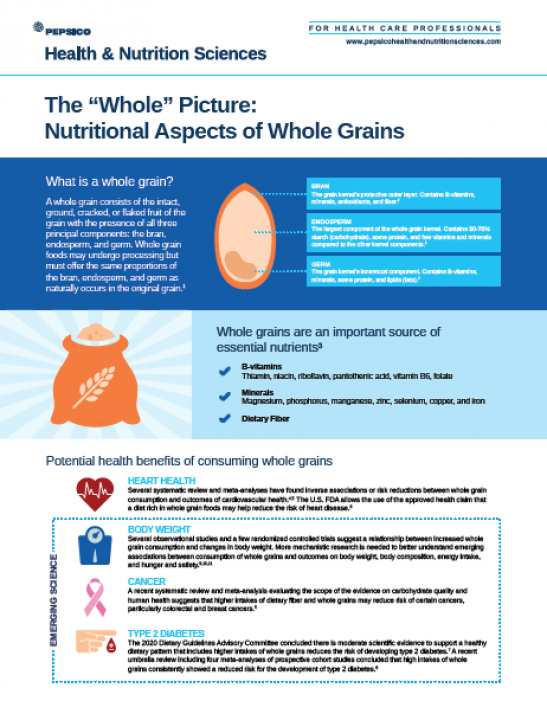
Mathews, R., & Chu, Y. (2020). Global review of whole grain definitions and health claims. Nutrition Reviews, 78(S1), 98-106. doi:10.1093/nutrit/nuz055
Abstract:
Recommendations to increase whole grain consumption are part of dietary guidelines around the world. To assist consumers in meeting this recommendation, some countries, and health-promoting organizations, have defined qualifying criteria for a whole grain food for product labeling or health claims. Other countries have not yet developed similar guidelines. Existing whole grain definitions and health claims are reviewed here. While there appears to be increasing consensus for defining a whole grain, significant disparity exists in defining a whole grain food when a product is not 100% whole grain. Moreover, while whole grain health claims have been approved in a few countries, other countries have concluded there is insufficient evidence to substantiate such claims.
Joyce, S. A., Kamil, A., Fleige, L., & Gahan, C. G. M. (2019). The cholesterol-lowering effect of oats and oat β-glucan: Modes of action and potential role of bile acids and the microbiome. Frontiers in Nutrition, 6, 171. doi:10.3389/fnut.2019.00171
Abstract:
Consumption of sufficient quantities of oat products has been shown to reduce host cholesterol and thereby modulate cardiovascular disease risk. The effects are proposed to be mediated by the gel-forming properties of oat β-glucan which modulates host bile acid and cholesterol metabolism and potentially removes intestinal cholesterol for excretion. However, the gut microbiota has emerged as a major factor regulating cholesterol metabolism in the host. Oat β-glucan has been shown to modulate the gut microbiota, particularly those bacterial species that influence host bile acid metabolism and production of short chain fatty acids, factors which are regulators of host cholesterol homeostasis. Given a significant role for the gut microbiota in cholesterol metabolism it is likely that the effects of oat β-glucan on the host are multifaceted and involve regulation of microbe-host interactions at the gut interface. Here we consider the potential for oat β-glucan to influence microbial populations in the gut with potential consequences for bile acid metabolism, reverse cholesterol transport (RCT), short-chain fatty acid (SCFA) production, bacterial metabolism of cholesterol and microbe-host signaling.
Olson, A., Frankenfeld, C. L., Wallace, T. C., & Johnson, J. (2018). Assessment of oats and milk on markers of cardiovascular disease: National Health and Nutrition Examination Survey 1999-2014 data sets. Nutrition Today, 53(6), 293-299. doi:10.1097/NT.0000000000000308
Abstract:
Background: Oat consumption has been suggested to decrease the risk of cardiovascular disease; oats are frequently co-consumed with milk, but also water and other products. Methods: We evaluated associations of 24-hour self-reported oat and cow’s milk consumption with cardiovascular disease risk factors using National Health and Nutrition Examination Survey (1999–2014) data. Daily oat and milk consumptions were classified as (1) no oats, no milk; (2) yes oats, no milk; (3) no oats, yes milk; or (4) yes oats, yes milk. We used no oats/no milk as a reference to assess the effects of oats, milk, and oat with milk consumption on markers of cardiovascular disease (CVD). The yes oats/no milk group was then used as the reference to further determine if a relationship between oat and milk consumption on the same day existed past that of previously reported oat consumption alone. Results: Self-reported oat intake was associated with improvements in some biomarkers of CVD risk. The prevalence of abdominal obesity measured as waist circumference was lower (odds ratio, 0.57; 95% confidence interval, 0.41–0.73), and fewer than 3+ risk factors of metabolic syndrome (odds ratio, 0.66; 95% confidence interval, 0.51–0.85) were observed in the yes oats/yes milk group as compared with nonconsumers (no oats/no milk). Similar effects were found in the yes oats/no milk group. We did not find any synergistic effects of self-reported consumption of both milk and oats during a 24-hour period on markers of CVD. Conclusions: These results are consistent with clinical data showing oats to be associated with improvement in some biomarkers of CVD risk; however, the addition of milk does not appear to affect CVD risk factors in this cross-sectional data set.
Earnshaw, S. R., McDade, C. L., Chu, Y., Fleige, L. E., & Sievenpiper, J. L. (2017). Cost-effectiveness of maintaining daily intake of oat β-glucan for coronary heart disease primary prevention. Clinical Therapeutics, 39(4), 804-818.e3. doi:10.1016/j.clinthera.2017.02.012
Abstract:
Purpose Oat β-glucan reduces cholesterol levels and thus reduces the risk for coronary heart disease (CHD). However, its economic impact has not been well studied. We examined the economic impact of daily intake of ≥3 g of oat β-glucan in primary prevention of CHD in patients receiving statins or no pharmacologic treatment. Methods A decision model was developed to compare costs and outcomes associated with lowering cholesterol levels with no pharmacologic treatment and normal diet, no pharmacologic treatment plus ≥3 g/d of oat β-glucan, and statin therapy plus ≥3 g/d of oat β-glucan. The population comprised men 45, 55, or 65 years of age with no history of cardiovascular disease and a 10-year risk for CHD of 5%, 7.5%, or 10%. Clinical efficacy data were gathered from meta-analyses; safety data, costs, and utilities were gathered from published literature. Cost per quality-adjusted life years and number of first events were reported. Findings Maintaining ≥3 g/d of β-glucan may be cost-effective in men aged 45, 55, and 65 years with 10-year CHD risks of 5.0%, 7.5%, and 10.0% taking no pharmacologic treatment or on statins. It may also reduce first events of myocardial infarction and CHD death. Results are sensitive to oat β-glucan cost but insensitive to changes in other parameters. Maintaining ≥3 g of oat β-glucan daily remains cost-effective within plausible range of values. Implications β-glucan may be cost-effective for preventing CHD events in middle-aged men with no history of cardiovascular events whose 10-year CHD risk is ≥5%. Maintaining daily β-glucan intake may have considerable impact on first events.
Gulati, S., Misra, A., & Pandey, R. M. (2017). Effects of 3 g of soluble fiber from oats on lipid levels of Asian Indians - A randomized controlled, parallel arm study. Lipids in Health and Disease, 16, 71. doi:10.1186/s12944-017-0460-3
Abstract:
Background Cardiovascular diseases are more prevalent and severe in Asian Indians. Simple diet-based strategies are important for prevention of cardiovascular diseases. The aim of the present study was to evaluate the effects of oats consumption on lipid parameters in mildly hypercholesterolemic Asian Indians living in India. Methods A short-term, prospective, open-labeled, randomized controlled, parallel group study was conducted. Mildly hypercholesterolemic (total cholesterol >200 mg/dL and <240 mg/dL) subjects (n = 80) were randomized into two groups: intervention (n = 40) and usual diet (n = 40). Sample size was calculated for a two-group parallel superiority randomized control trial. Out of 80 enrolled subjects 69 subjects completed the study; 33 in the control group and 36 in the intervention group. In the intervention group, patients were served 70 g of oats twice a day in the form of porridge and upma (A thick porridge from oats with seasonings and vegetables) under observation at the study site. Lipid parameters were assessed at baseline and after 4 weeks of intervention. Results There was a reduction of 3.1% in total cholesterol levels in the control group as against 8.1% reduction in the intervention group (p < 0.02). Greater reductions were also seen in low-density lipoprotein cholesterol in the intervention group (11.6%) as compared to control group (4.1%, p < 0.04) over a period of 28 days. Conclusion Daily consumption of 3 g of soluble fiber from 70 g of oats leads to beneficial effects on the lipid parameters, specifically total cholesterol and low-density lipoprotein cholesterol in hypercholesterolemic Asian Indians. Large scale studies over a longer period of intervention are required to further establish the cholesterol-lowering effect of oat fiber.
Zhang, J., Li, L., Song, P., Wang, C., . . . Kurilich, A. (2012). Randomized controlled trial of oatmeal consumption versus noodle consumption on blood lipids of urban Chinese adults with hypercholesterolemia. Nutrition Journal, 11, 54. doi:10.1186/1475-2891-11-54
Abstract:
Background Cardiovascular disease (CVD) is the leading cause of death in China and worldwide. Whole grain oats can reduce risk of CVD by reducing total and LDL-cholesterol, major risk factors for CVD. While this association has been established in many populations, data from Asian populations is limited. Thus, this study investigated the impact of oat consumption on cholesterol levels in Chinese adults. Male and female data from this work were previously published separately in mandarin in two Chinese journals. The combined male and female data were reanalyzed and are presented here. Methods A randomized, controlled, parallel-arm study was conducted at Beijing Hospital, Beijing china. Subjects were adults (men and women) with mild to moderate hypercholesterolemia. The oat group (n=85) consumed 100grams of instant oat cereal versus the control group (n=81) who consumed 100grams of wheat flour-based noodles daily for 6weeks. Laboratory and anthropometric measurements were conducted at baseline and at the end of the 6-week intervention. Results Dietary fiber intake increased significantly in the oat group compared to the control group at the end of the 6-week intervention. Total-, LDL-cholesterol and waist circumference decreased significantly in the oat group compared to the control. HDL-cholesterol decreased significantly in the control group versus the oat group. There were no significant changes in blood pressure, other anthropometric or laboratory measures between the two groups at the end of the intervention. Conclusions Instant oatmeal consumed daily for 6 weeks significantly increased fiber intake and decreased major risk factors for CVD in Chinese adults with hypercholesterolemia. Increased consumption of whole grains, including oats, should continue to be encouraged.
Rendeiro, C., Dong, H., Saunders, C., Harkness, L., . . . Spencer, J. P. E. (2016). Flavanone-rich citrus beverages counteract the transient decline in postprandial endothelial function in humans: A randomised, controlled, double-masked, cross-over intervention study. British Journal of Nutrition, 116(12), 1999-2010. doi:10.1017/S0007114516004219
Abstract:
Specific flavonoid-rich foods/beverages are reported to exert positive effects on vascular function; however, data relating to effects in the postprandial state are limited. The present study investigated the postprandial, time-dependent (0–7 h) impact of citrus flavanone intake on vascular function. An acute, randomised, controlled, double-masked, cross-over intervention study was conducted by including middle-aged healthy men (30–65 years, n 28) to assess the impact of flavanone intake (orange juice: 128·9 mg; flavanone-rich orange juice: 272·1 mg; homogenised whole orange: 452·8 mg; isoenergetic control: 0 mg flavanones) on postprandial (double meal delivering a total of 81 g of fat) endothelial function. Endothelial function was assessed by flow-mediated dilatation (FMD) of the brachial artery at 0, 2, 5 and 7 h. Plasma levels of naringenin/hesperetin metabolites (sulphates and glucuronides) and nitric oxide species were also measured. All flavanone interventions were effective at attenuating transient impairments in FMD induced by the double meal (7 h post intake; P<0·05), but no dose–response effects were observed. The effects on FMD coincided with the peak of naringenin/hesperetin metabolites in circulation (7 h) and sustained levels of plasma nitrite. In summary, citrus flavanones are effective at counteracting the negative impact of a sequential double meal on human vascular function, potentially through the actions of flavanone metabolites on nitric oxide.
Slimko, M. L., & Mensah, G. A. (2010). The role of diets, food, and nutrients in the prevention and control of hypertension and prehypertension. Cardiology Clinics, 28(4), 665-674. doi:10.1016/j.ccl.2010.08.001
Abstract:
Hypertension is the leading risk factor for death worldwide, even surpassing tobacco use, high blood glucose, high blood cholesterol, and obesity. Globally, the estimated prevalence of hypertension is nearly 1 billion persons with an annual mortality of almost 7.5 million deaths. In the United States, hypertension affects an estimated 65 million Americans, and it is the leading risk-factor cause of death in women and only second to tobacco use as a contributory cause of death in men. Multiple sources of data from prospective observational, cohort, and randomized controlled clinical trials show that hypertension and its complications are highly preventable when the raised blood pressure (BP) is prevented, or treated and controlled. In fact, average reductions of just 5 to 6 mm Hg of diastolic BP in large, randomized, placebo-controlled trials resulted in an approximate reduction of 38% in stroke, 16% in incident coronary heart disease events, 21% in composite cardiovascular events, and 12% in death from all causes. A fundamental component of effective prevention, treatment, and control of hypertension is the adoption of recommended behavioral and lifestyle changes among which dietary intake of foods and nutrients play crucial roles. In this article, the authors focus on the role that diet, foods, and nutrients play in the prevention and control of hypertension and prehypertension. The report of the 2010 Dietary Guidelines Advisory Committee (DGAC) is reviewed, and its recommendations relevant to the promotion of nutrition education and the prevention and control of hypertension are summarized. The role of the dietitian, as a critical member of the care team for the management of hypertension, is also discussed. Finally, the role of the food system, including food manufacturers and restaurants, in addressing dietary sodium intake, calorie density, and other strategies in support of energy balance to support the prevention and control of hypertension and prehypertension is discussed.